Worsening Cardiovascular Disease Epidemiology in the United States: The Time for Preparation Is Now
The ongoing COVID-19 pandemic has challenged health care systems worldwide and has brought to the forefront the limitations of providing high-quality health care under system stress. However, in many instances, COVID-19 was more of a trigger to expose the vulnerabilities of the chronically stressed primary and specialty health care system in the United States. The burden of the pandemic on health care providers has had a profound effect on both hospital and outpatient clinician workforces, and many of these effects are projected to persist.However, concerns with shortages and maldistribution of the health care workforce in the United States preceded the pandemic. In a report by the Association of American Medical Colleges in June 2020, with data derived from surveys conducted before the pandemic, a primary care physician shortage of between 21,400 and 55,200 was projected by the year 2033, whereas the corresponding projection for nonprimary care, specialty physicians was in the range of 33,700 to 86,700. Similarly, notwithstanding the multifaceted impact of the pandemic on cardiovascular care, with direct allocation of resources to the care of patients with COVID-19 and the indirect effects of other pandemic-related disruptions, problems with the supply and demand of the cardiovascular workforce were evident long before the pandemic.
With this health care landscape as backdrop, Mohebi et al, in this issue of the Journal of the American College of Cardiology, project the prevalence of cardiovascular risk factors and cardiovascular disease in the United States from 2025 to 2060. For this purpose, Mohebi et al, combined the projections on population growth and demographic distribution from the U.S. Census Bureau report in 2020 with data on the prevalence of cardiovascular risk factors and cardiovascular disease from the 2013-2018 U.S. National Health and Nutrition Examination Survey (NHANES), according to demographic subgroup. Appropriate regression models were applied to consider the sampling design of NHANES and adjust for age, sex, race, ethnicity, and survey years. Even though several assumptions underlie these projections, the importance of this work cannot be overestimated. The absolute numbers are staggering and suggest that by the year 2060, compared with 2025, the numbers of people with diabetes, hypertension, dyslipidemia, and obesity are projected to increase by 15.4, 34.7, 27.1, and 19.4 million, respectively. The corresponding projected increases in patients with prevalent ischemic heart disease, heart failure, myocardial infarction, and stroke are 6.8, 3.2, 3.7, and 3.7 million, respectively. Although the total number of White persons with cardiovascular risk factors and disease is projected to decrease over time, significant increases in the corresponding numbers are projected among racial and ethnic minority groups. On the basis of these findings, the projected stresses on both primary care and specialty care have important implications for public health, health care, and medical education policies.
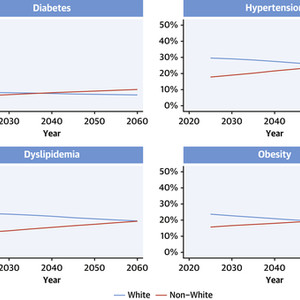
A striking finding by Mohebi et al is that the total number of individuals with cardiovascular risk factors among racial and ethnic minority groups is projected to surpass the corresponding White individuals over time (Figure 1A), and the total number of patients among Hispanic, non-Hispanic Black, and other non-Hispanic racial and ethnic groups with cardiovascular disease will be almost as many as White patients by the year 2060 (Figure 1B). From a policy perspective, this means that unless appropriate, targeted action is taken, disparities in the burden of cardiovascular disease are only going to be exacerbated over time. On the positive side, the absolute increase in the percent prevalence of cardiovascular risk factors and conditions is projected to lie within a manageable range (Figures 2A and 2B). Manageable, however, assumes that we implement specific policies to prevent the incidence of cardiovascular risk factors (primordial prevention), control prevalent risk factors (primary prevention), and limit the impact of manifest disease (secondary prevention). These assumptions are fragile, however, because they require addressing lifestyle education at the public health level and tackling access issues for both primary care and cardiovascular care. For example, although recent data suggest that the prevalence and control of some cardiovascular risk factors in the United States has been declining between years 1999 and 2018 in the total population, with a corresponding decrease in projected cardiovascular disease risk, the decline was not proportional across demographic subgroups.


Projected Prevalence of Cardiovascular Risk Factors and Conditions According to Race
Demographic distribution of cardiovascular disease burden is important for prevention efforts. On the basis of data from the 2020 U.S. Census Bureau report and demographic-specific data from the 2013-2018 U.S. National Health and Nutrition Examination Survey (NHANES), Mohebi et al4 have projected the prevalence of (A) cardiovascular risk factors and (B) conditions for the years 2025-2060 in the United States. According to these projections, the number of individuals from minority communities (red lines) with cardiovascular risk factors is projected to surpass those of White race or Caucasian heritage (blue lines) over time, as a percentage of the total U.S. population. The number of minority patients with cardiovascular disease will be almost as high as that of White or Caucasian patients by the year 2060. Non-White = Hispanic, non-Hispanic Black, and other non-Hispanic racial and ethnic groups. Data from Mohebi et al.

Projected Population Prevalence of Cardiovascular Risk Factors and Conditions
The cumulative burden of cardiovascular disease is important for health care policy and planning. Using the methodology described in Figure 1, this graph summarizes the projected prevalence of (A) cardiovascular risk factors and (B) conditions for the years 2025-2060 in the total U.S. population. Despite the large increases in absolute numbers, partly because of growth and aging of the population, the increase in prevalence should be manageable with appropriate prevention and management policies. IHD = ischemic heart disease; MI = myocardial infarction. Data from Mohebi et al.
As Mohebi et al appropriately acknowledge, the trends in the prevalence of risk factors were not incorporated into the projections because it would be extremely difficult to predict trends in the demographic-specific prevalence of these risk factors (and the subsequent impact on incident cardiovascular disease) with reasonable accuracy until year 2060. Management of cardiovascular risk factors requires access to primary care, and diversity of the health care workforce may play a key role in this aspect. According to the 2020 Association of American Medical Colleges report, the demand for physician services is projected to grow from 2018 to 2033 by 9% among the non-Hispanic White population, whereas the corresponding growth among the Hispanic, non-Hispanic Black, and other non-Hispanic population will be 43%, 25%, and 39%, respectively. Therefore, if we use past trends as a guide, it is reasonable to assume that with aging of the population and uneven growth in health care services demands across racial and ethnic minority groups, these divergent trends in the management of cardiovascular risk factors are likely to continue unless we take targeted action. In this line of thought, training a physician workforce from diverse racial, ethnic, and socioeconomic backgrounds could be a solid step toward better primary care and prevention efforts. However, recent data suggest that we still need to do a lot of work in this direction.
Specifically for cardiovascular specialty care, what are the implications of the projections made by Mohebi et al? Considering these findings, it is worth revisiting the American College of Cardiology’s Fellow-In-Training Council 2016 report by Narang et al. The report considered several factors, including an aging cardiology community, limited growth in training positions, increasing burden of cardiovascular disease, and evolving health care reform, as main drivers of the supply and demand mismatch. We are recasting here the recommendations of the Council:
1. Emphasize cardiovascular disease prevention. Besides primary care considerations discussed earlier here, emphasize secondary prevention during cardiovascular training, for example, to prevent recurrent and new vascular events among patients with preclinical and clinical atherosclerotic disease (coronary, peripheral, cerebral), lower the risk of heart failure in patients with stage B disease, and prevent stroke in patients with atrial fibrillation.
2. Optimize the cardiovascular care team, by integrating input from every member of the team (eg, advanced practice nurses, dietitians, physical and occupational therapists, social workers) in the care of the patient.
3. Adapt the training of future cardiologists, including alternative (and potentially shorter for certain directions) training pathways, with an emphasis on the appropriate use of diagnostic and therapeutic procedures, and education on health care policies and reforms.
In summary, Mohebi et al bring to the forefront important challenges for our policies in cardiovascular disease prevention and caring for patients with cardiovascular disease in the decades to come. This is an opportunity for professional societies, including the cardiovascular care community, to re-evaluate priorities and strategies, for both training and practice, to best match the growing demands of a changing demographic landscape in the United States.
This article is reproduced from JACC journals.
surgerycast
Shanghai Headquarter
Address: Room 201, 2121 Hongmei South Road, Minhang District, Shanghai
Tel: 400-888-5088
Email:surgerycast@qtct.com.cn
Beijing Office
Address: room 709, No.8, Qihang international phase III, No.16, Chenguang East Road, Fangshan District, Beijing
contact number:13331082638(Liu Jie)